Limiting Late Effects Following a Transplant Using Donor Cells (Allogeneic)
Limiting Late Effects Following a Transplant Using Donor Cells (Allogeneic Transplant)
Saturday, May 3, 2025
Presenter: Dr. John McCarty, MD, Virginia Commonwealth University Massey Cancer Center
Presentation is 42 minutes with 14 minutes of Q & A
Many thanks to Sanofi, whose support helped make this presentation possible.
Summary: This presentation outlines the importance of long-term follow-up care after a bone marrow/stem cell transplant using donor cells (allogeneic transplant) focused on supportive care for side effects post-transplant, identifying new health issues early, and providing resources and guidance to ensure the patient is experiencing their optimal quality of life after treatment.
Key Points:
- There are many potential side effects and complications that someone may experience after a bone marrow/stem cell transplant.
- Preventive health maintenance is the key to optimal post-transplant health and requires a multidisciplinary team that frequently monitors all systems in the body..
- Patients can take charge of their health and well-being by being proactive in their care. Thorough communication with their providers, consistent exercise, prioritizing safe social interaction and relationships, and maintaining good psychological health are all effective ways to thrive after transplant.
(01:44): An allogeneic bone marrow/stem cell transplant is one of the most powerful immune therapies for cancer that we have at our disposal.
(09:15): Regular skin exams after transplant are important, and patients should be vigilant in limiting their sun exposure.
(12:13): There are protocols to follow to help re-establish a patient’s immunity against infections.
(17:09): Bone loss should be followed very closely.
(20:22): Patients should prioritize exercise after transplant.
(21:57): Sexual function can be an issue. It’s very common with certain chemotherapies – such as high-dose cyclophosphamide (Cytoxan) – and radiation – especially total body radiation.
(23:25): Infertility after transplant is not a certainty, but high-dose cyclophosphamide (Cytoxan) and total body radiation are associated with higher rates of infertility, and women are more impacted than men.
(24:21): Pulmonary problems caused by certain chemotherapies, radiation, and graft-versus-host disease can occur.
(32:44): Secondary cancers can arise, but while it's a higher risk than the general population, the incidence is still relatively low.
(35:33): About 75% of patients get back to their pre-transplant physical abilities and functioning levels around one year, and this is enhanced in those who have been consistent with exercise throughout treatment.
Transcript of Presentation.
(00:01): [Marla O'Keefe]: Welcome to the workshop, Limiting Late Effects Following a Transplant using Donor Cells. My name is Marla and I will be your moderator for this workshop.
(00:10): Before we begin, I'd like to thank Sanofi, whose support helped make this workshop possible.
(00:17): Introduction. It is my pleasure to introduce today's speaker, Dr. John McCarty. Dr. McCarty is the Medical Director of the Cellular Immunotherapy and Transplant Program at Virginia Commonwealth University Massey Cancer Center in Richmond, Virginia, and the Medical Director of the Cellular Therapeutics Laboratory. His clinical work focuses on treating patients who have leukemia, multiple myeloma, lymphoma, myeloproliferative syndrome, or bone marrow failure disease. He also specializes in cellular immunotherapies for autoimmune diseases. Please join me in welcoming Dr. McCarty.
(01:01): [Dr. John McCarty]: Thank you for that very kind introduction. I'm very pleased to be part of this excellent symposium that provides so much supportive information to patients that have been through or are considering transplant, caregivers, and other providers who support our work in transplant and cellular therapy.
(01:23): Overview of Talk. I will be speaking to you this afternoon about not just surviving an allogeneic transplant, but about what we can do to allow survivors to thrive and really excel in their quality of life after undergoing an allogeneic transplant.
(01:44): An allogeneic bone marrow/stem cell transplant is one of the most powerful immune therapies for cancer that we have at our disposal. The first thing I want to discuss is what an allogeneic transplant is. It differs from other kinds of transplants and cellular therapies as we’re using blood cells from a related family member, an unrelated donor, or potentially even an umbilical cord blood donor to do the transplant. We can collect these cells from a donor’s bone marrow or peripheral bloodstream, or use banked umbilical cord blood.
(02:18): It's much more than just giving someone clean bone marrow; they are receiving a brand-new immune system. The cells from the donor are moving into their body and are going to be less tolerant of the cancer that’s being treated.
(02:35): I often give my patients this analogy; It's almost as if your donor moves into your body – into ‘a new house’ – looks around and says, "Nice house, I can live here." But it's going to want to do some renovation. And the main thing it wants to do is to look at that bone marrow, or look at that leukemia or lymphoma or myeloma or whatever we're treating, and want to reject that cancer. Because of this, an allogeneic transplant is one of the most powerful immune therapies for cancer that we have at our disposal.
(03:11): There are many different steps involved in undergoing an allogeneic bone marro/stem cell transplant. First, you need to have chemotherapy, called a preparative or conditioning regimen. The purpose of this regimen is to create space in the bone marrow for the new cells to be able to take hold, and to suppress the recipient's own immune system to allow the new immune system from the donor to move in and begin functioning.
(03:37): The donor cells are then infused intravenously, where they circulate in the recipient’s blood stream, make their way into the bone marrow, and begin proliferating and growing.
(03:46): The recipient will take immunosuppressive medications – or medications that suppress the recipient’s immune system – to prevent rejection of the donor cells, and to prevent the donor cells from potentially reacting against more than just the cancer. The duration and types of these medications are individualized to the patient, the type of transplant, and the form of donor cells being used.
(04:07): After a transplant, there is a long period of time where the immune system is suppressed and weak, so many lifestyle changes need to take place in order to reduce the risk of infections and complications. Patients also continue taking immunosuppression medications in order to reduce the risk of graft-versus-host disease, which is caused by an over reactivity of the donor cell’s immune response against the cancer.
(04:35): More and more transplant programs are setting up long-term follow-up programs and survivorship clinics, as post-transplant care is very important. We actually started a long-term follow-up clinic here at Virginia Commonwealth University (VCU) Massey Cancer Center more than 15 years ago. While it includes transplant physicians, nurse practitioners, and physician assistants, it also includes transplant-focused physicians and specialists in psychology, psychiatry, endocrine, pulmonary, kidney diseases, infectious diseases and so on. This ensures the patients are continuing to be followed by a multidisciplinary team, and receiving supportive care for issues that may arise.
(05:31): While it is very individualized, a patient can expect their follow-up care to continue for at least 10 years. Generally, the focus and goals within the follow-up care change over time. Initially, especially for the first two years, we are focusing on their disease status and if they are staying in remission. Relapse typically occurs in the first five years, and throughout that time, we may be using certain treatments to help prevent relapse. We are also preventing, diagnosing, monitoring and treating any graft-versus-host disease (GVHD) and assessing if treatments that enhance or improve their immune system are needed.
(06:32): After that, our focus shifts to maintaining the overall health of the patients, focusing on all organ systems in the body. Some of this will occur in the transplant program, or long-term follow-up clinics, but this will also be a partnership between multiple transplant-focused physicians, specialists, and your oncologist.
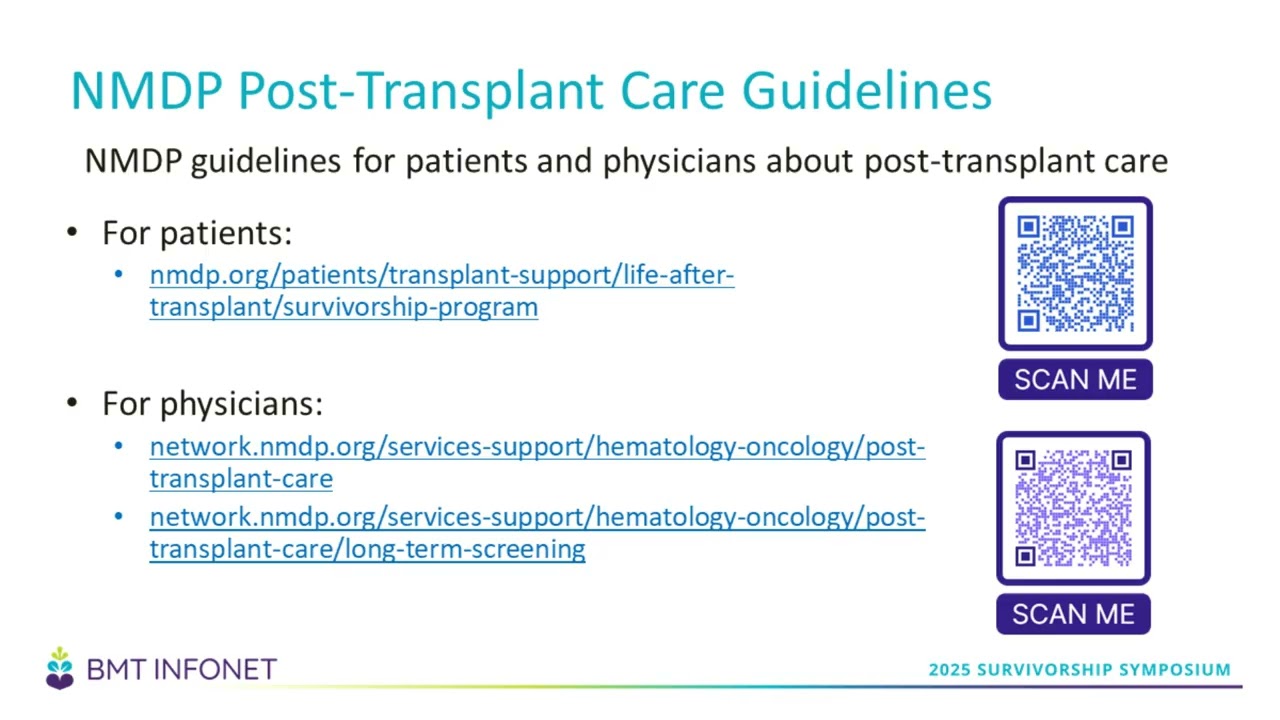
(07:03): The National Marrow Donor Program (NMDP) has put together a number of guidelines for post-transplant care. There are guidelines for both patients and physicians. On the slide, you can see the website address and QR codes that link to those resources.
(07:30): There are some long-term complications related to treatment with chemotherapy and transplant. These complications depend on many factors including, the specific type of chemotherapy the patient received, if they received radiation and where, and the dosage of chemo or radiation used. Metabolic and endocrine health may be affected. The strength of the immune system will be affected and the patient will have an increased risk of infections. There are long-term impacts on fertility, heart and lung health, and even a small risk of secondary cancer related to the treatments they received.
(08:09): Long-term care also focuses on how well a patient is reintegrating back into their life after treatment. It ensures their social life, ability to function at work, and home life are back to a level of satisfaction that is sustainable, and adding to a healthy and happy quality of life.
(08:27): Long-term health screenings are also recommended, as there are things we can monitor to try to identify issues early, and prevent future health problems. Doing regular cardiovascular screening, monitoring your blood pressure, checking your lipids – your cholesterol and triglycerides – often, and monitoring your blood sugar, are all things we can monitor to ensure you are staying healthy. Health issues that occur as we age may be associated with different risks post-treatment, and while your cancer may now be cured, we don't want these other health issues to affect your quality and quantity of life.
(09:15): Skin exams are also important, and patients must be vigilant in limiting their sun exposure. Skin that has been exposed to chemotherapy or radiation, or patients taking antibiotics or receiving other treatments, are at increased risk of sunburn and sun injury. We recommend that patients get annual skin exams, and if they have a history of sun damage or skin cancers, then more frequently, as recommended by their dermatologist.
(09:53): In regards to monitoring the endocrine system – which impacts energy levels, hormones and really a general state of well-being – we recommend annual testing. We look at the thyroid function, testosterone and estrogen levels, as well as the hemoglobin A1C – which is a measure of your long-term average glucose control. The patient’s individual risk and treatment plan may indicate more frequent monitoring, but at a minimum, patients can expect annual screenings for these things.
(10:29): We monitor the gastrointestinal (GI) tract in many ways. Specifically with the liver, we will perform annual liver function tests. If someone has increased risk factors prior to transplant –such as a history of cirrhosis, hepatitis B, or hepatitis C – we make sure these are not reactivated. Likewise, in patients that have had a large number of blood transfusions, iron overload can have an impact on the liver as well. Regardless of the patient’s history, we will always do blood tests, including a complete blood count (CBC), at each visit for at least 10 years to ensure complications like iron overload are not occurring. Patients experiencing graft-versus-host disease involving the liver will need to be followed even more closely and more often.
(11:27): The musculoskeletal system is also closely monitored. People with chronic graft-versus-host disease may have some thickening and tightening of the connective tissue or the skin over their joints, leading to decreased range of motion and stiffness. Early identification and intervention is key, and doing regular exercises – not just strength training but with a focus on range of motion and flexibility – is critical to help limit these issues.
(12:13): There are protocols to follow to help re-establish a patient’s immunity against infections. After an allogeneic transplant, we have completely erased your entire immune system, so any vaccinations and immunities that your body previously had are now gone. Beginning at 3 to 6 months post-transplant, patients can expect to receive vaccinations for COVID and flu, pneumonia, and meningitis. Hepatitis, diphtheria, tetanus and polio, mumps, measles, rubella, and shingles vaccinations are also all appropriate and administered at specific times.
(12:55): There are many vaccination protocols, and this is something I would check with your transplant physician and long-term follow-up team to determine when these should happen. A national study with the Center for International Blood and Marrow Transplant Research was done on the COVID and flu vaccines, and the study determined it safe and beneficial to administer those vaccines starting at day 100 after transplant.
(13:32): Your antibody levels may be low while your immune system is trying to recover, which is called ‘hypogammaglobulinemia’. In most cases after transplant, you will be on preventative antibiotics, antivirals and antifungals until your immune system is more intact and robust. If you've had graft-versus-host disease, some of the immune suppression medications will further impact and weaken your immune system. Doctors may consider giving you a bag of plasma or intravenous immunoglobulin (IVIG) if your immunoglobulin levels are under 400 milligrams per deciliter (mg/dL). This has been shown to not only boost the immune system, but reduce the severity and incidence of sinus and pulmonary infections.
(14:28): Vision screenings and eye exams are also a part of long-term follow-up care. Graft-versus-host disease (GVHD) of the eyes can cause a variety of symptoms including dry eyes, bloodshot eyes, and excessive tearing. It's important to have an ophthalmologist – especially one who is familiar with transplant patients – check for and evaluate these symptoms. Radiation, graft-versus-host disease, and long-term steroid exposure, can cause an increased risk of cataracts, so annual ophthalmology exams are important.
(15:26): Treatments including chemotherapy, antibiotics, and immune suppression medications can sometimes interfere with kidney function, either temporarily or long-term. At a minimum, annual kidney function tests are important.
(15:51): We recommend having regular gynecological (GYN) exams as well. This is true for both people who are premenopausal or postmenopausal. Patients can experience graft-versus-host disease of the vulvar and vaginal area, so continuing to monitor in all stages of the transplant process is important. Not everyone can get the Gardasil vaccination to protect against the human papillomavirus (HPV), that has been associated with cervical cancer. During the period of immunosuppression or when the immune system may not be completely normal, that could be an opportunity for that virus to reactivate and potentially lead to cervical dysplasia, which can be treated effectively if it's caught early.
(17:06): Mammography is also very important, especially for women who have had radiation therapy. Maintaining your health and staying on track with usual appointments are very important. Remember, you did the transplant to maintain excellent health, so let's make sure nothing else happens.
(17:09): Bone loss is something we follow very closely. Avascular necrosis is a condition in which the bone loses some of its blood supply, deteriorates and can collapse. It only happens in about 5 to 10% of patients and it's usually associated with very prolonged or high-dose uses of corticosteroids – like prednisone or methylprednisolone. It commonly occurs in the hips, and less often in the ankles and shoulders. We see an increased risk for avascular necrosis in patients doing gene therapy or transplant for sickle cell disease – which may actually be more related to their history of sickle cell – that persists or worsens during transplant. Immunosuppressive medications including cyclosporine, tacrolimus, and sirolimus, can contribute to bone loss and bone thinning. Being sedentary is another significant risk factor for bone loss. Bone thinning can occur in 50% to 60% of patients. 20% of these people will actually progress to true osteoporosis, and 1% to 5% may develop symptomatic fractures. Those may not seem like big numbers, but if it happens to you, it's a pretty significant thing.
(18:38): Other risk factors for bone loss include a family history of these complications, and increases the chances of severity. Patients who experience a loss of testicular function or ovarian endocrine function as a result of chemotherapy have an increased risk, because estrogens and testosterone are actually protective against bone loss. Prolonged use of growth factors to treat low blood counts occasionally contribute to some bone loss as well. If the kidneys are not functioning properly, their role in managing calcium storage and bone health can be impaired, and may be a contributory factor.
(19:24): To monitor and prevent this, bone density testing can be done every two years. If someone is at risk or diagnosed with osteoporosis, there are medications that are used post-transplant to help with calcium absorption and bone density. Testing calcium and vitamin D blood levels are important, and supplementing if necessary. Hormone replacement therapy may be used in both men and women to help prevent bone loss, although the risks and benefits of this must be individualized for each patient and discussed with a provider. For example, someone who has a history or increased risk of breast cancer should look at different options to prevent the risk of reactivation or recurrence.
(20:22): Patients should prioritize exercise. I can’t emphasize enough how important exercise is, and patients should be exercising in all stages of treatment – before, during, after chemo and after transplant. We're not looking for people to beat Usain Bolt at the next Olympics. You want to focus on core activities, such as yoga, Tai Chi, and Pilates. You can do Richard Simmons and Jane Fonda if you’d like, but you don't have to do it as fast as they do. It's time-focused and scaled to your energy levels, with a goal of at least 30 to 40 minutes a day. Activities to improve cardiovascular health include walking, treadmill, exercise bike, and elliptical. If you happen to have children or grandchildren who have a gaming system, some of them even have exercise programs. Even playing ‘Just Dance’ or ‘Dance, Dance Revolution,’ is a core, cardiovascular-focused exercise. Make it fun, mix it up, and commit to doing one of those exercises every day, for the rest of your life. It has a very important impact in preventing bone loss.
(21:57): Sexual function can be an issue. It’s very common with certain chemotherapies – such as high-dose cyclophosphamide (Cytoxan) – and radiation – especially total body radiation. Both males and females can go through a version of menopause, and hormonal changes can impair sexual function. The vaginal mucosa may become thin – which is actually a risk factor for vulvar or vaginal graft-versus-host disease – and experience decreased lubrication, which can both lead to very painful sexual function. Treatment can also reduce the flexibility or stability of the pelvic floor, leading to problems with incontinence and other issues. Low testosterone may be associated with lower libido. Hormone replacement treatments really need to be discussed with your doctors, and it takes a multidisciplinary approach. For example, estrogen replacement is not the only option necessarily, and sometimes an estrogen cream given intravaginally is enough to reduce a lot of these issues.
(23:25): Fertility planning and potential challenges are also considered. Infertility is not a certainty, and many patients have been able to recover their fertility after treatment. High-dose cyclophosphamide (Cytoxan) and total body radiation are associated with higher rates of infertility, and women are more impacted than men. We often talk about sperm and egg banking prior to transplant as an option to be pursued for people who would still like to have children after the transplant process. You can learn more about building a family after transplant by watching a video on BMT InfoNet's website at bmtinfonet.org/video/building-family-after-transplant-0.
(24:21): Pulmonary scarring (scarring in the lungs) can occur with certain chemotherapies, and from radiation scatter if areas of the chest or neck were targeted. A condition called ‘engraftment pulmonary inflammation’ can sometimes occur when the cells are engrafting, and the immune system causes some injury to the lungs. Those who have previously smoked or had some other prior inflammation in the lungs, are at increased risk. This can effectively be treated if identified early.
(25:06): Lungs can also develop graft-versus-host disease. Identifying it early and working with a bone marrow transplant-focused pulmonologist to treat this is very important to preserve as much lung function as possible. Sometimes, if an area of the lung has been irradiated because of prior breast cancer or lung cancer, that area of the lung may not be as functional anymore. Complications such as graft-versus-host disease or infections, can cause issues such as the lining around the lungs to become thickened, or even adhere together. Fluid can collect around the lungs that might compress them and decrease lung function. Some people actually have to have surgery on their lungs, such as removing a portion of a lung affected by a fungal infection.
(26:35): Within your follow-up care, we will perform pulmonary function tests and high-resolution computed tomography (CT) scans for at-risk patients. We want to jump on any inflammatory pneumonia or pneumonitis (inflammation of the lung) that we might see. Reporting any changes in exercise tolerance is a useful way to help identify new issues that may be arising. Whenever the pulmonary function tests show even an asymptomatic decrease of 10%, we often start a protective therapy and send patients to the pulmonologist to be followed to ensure that we're preventing any further lung injury.
(27:17): It is crucial to not resume smoking, vaping, or be around secondary smoking. This also includes using wood-burning fires or wood-burning ovens. If you can stop smoking before you get to transplant, and not start up again, this will set you up well for maintaining good pulmonary health.
(28:16): Radiation, chemotherapy and hormonal changes can increase the risk of heart problems after transplant. Heart attacks have been seen after chest radiation specifically, but not total body irradiation. Estrogen levels in the blood are actually protective against cardiac disease, so hormonal changes add to an increased risk of heart attack. Going into transplant, some people may develop, or already have, a group of conditions called ‘metabolic syndrome’ that can increase your risk, as well as ‘insulin resistance’--or sometimes called ‘adult-onset diabetes.’ High blood pressure, high lipids, and abdominal obesity also add to that risk.
(29:10): Some of the chemotherapies can cause congestive heart failure, such as anthracyclines – which isn’t typically used in transplant, but may have been administered beforehand in your prior treatment. Less than 5% of patients who received cyclophosphamide (Cytoxan) or melphalan, during their transplant chemotherapy regimen, may be at risk for congestive heart failure as well.
(29:29): VCA has a cardio-oncology service, and many other centers are also establishing this specialty to help with these unique issues and needs. A regular cardiologist may not fully understand what's needed to clear patients for transplant, or how to maintain, monitor, and optimize treatments afterwards. We've had a cardio-oncology service for almost 10 years to meet the unique needs of cancer patients. Attend your regular, recommended cardiology checkups, and report any changes in your overall health. Report any small change or anything different that you are noticing. You are the best person to know how you feel. We'd rather hear about changes and find out it's nothing, rather than waiting and wishing we had intervened earlier.
(30:29): Immune reconstitution – or recovering your immune system after transplant – is another focus and treatment component post-transplant. We already discussed how common having lower immunoglobulin levels, and therefore a higher risk of infection, is. The spleen, which helps filter the blood of certain infections, may also be reduced in function. Preventative antibiotics are key in helping reduce infections as we wait for the immune system to heal.
(31:03): Graft-versus-host disease may delay when the immune system becomes fully functional again. Some people may need long-term antibiotics to prevent pneumococcal pneumonias. Shingles can reactivate in 20% to 50% of patients, so we prescribe the antiviral acyclovir, to prevent this and administer the shingles vaccine once the immune system is back to normal. There's a type of pneumonia called pneumocystis jiroveci pneumonia (PJP) that can occur up to a year post-transplant. Very often, you remain on various treatments to prevent infection, until your immune system is strong enough to prevent infections.
(31:50): As previously discussed, re-vaccination starts around 3 to 6 months after transplant. I've talked about the study looking at the COVID and flu vaccine, because those can cause very significant infections. I also recommend that caregivers are fully vaccinated because in our experience, 85% of COVID and flu infections come from close contact with family members. The Center for International Blood and Marrow Transplant Research has a link on their website that displays the post-transplant vaccination guidelines at bit.ly/CIBMTR-Post-Transplant-Guidelines.
(32:44): Secondary cancers can arise, but while it's a higher risk than the general population, the incidence is still relatively low. The cumulative incidence at 15 years is no more than 10% to 12%. It's incredibly uncommon and it's usually related to chemotherapy treatment as well as certain infections. Epstein-Barr virus can lead to lymphoma. Hepatitis C can potentially lead to liver cancer. Human papillomavirus can lead to cervical cancer. These all may arise at different times.t we look for these are different. Lymphoma arising from the Epstein-Barr virus may occur the first 100 days to one-year post-transplant. On average, secondary blood cancers will occur within the first five years. Secondary solid tumors occur much later -- anywhere from 10 to 30 years or longer after transplant. This is another reason why we stay in touch with your doctors and continue to follow up.
(34:15): There is a 4%-5% incidence for leukemia and blood cancers, and they usually occur within the first year of transplant if it's going to occur. These are associated with very focused radiation therapy, or the use of certain chemotherapies, typically not the ones we use in transplant, but ones you may have received prior. We've also seen that if we transplant with an inadequate number of stem cells per kilogram of your body weight, that can increase the risk, and to a smaller degree, total body radiation or radiation can increase that risk. For solid tumors, skin cancers, breast cancer, oral cancers, and central nervous system cancers, have a cumulative incidence rate of about 6% to 11% at 15 years.
(35:03): Younger patients who are under the age of 10 and have had a transplant have the highest risk of developing secondary cancers. This is due to the immunosuppressive medications, radiation, graft-versus-host disease, and other viral infections that may have been experienced during their treatment.
(35:14): Health maintenance, and making sure that all of your physicians are in communication and have a health summary from the transplant team, are ways you can ensure you are doing everything you can to stay as healthy as possible.
(35:33): About 75% of patients get back to their pre-transplant physical abilities and functioning levels around one year, and this is enhanced in those who have been consistent with exercise throughout treatment. 85% of people return to work or school, and only about 25% have any kind of physical limitations that might affect their ability to work after treatment. Usually, these are patients experiencing persistent graft-versus-host disease.
(36:06): The people who do best are those who have good psychological health. You can have good psychological health by maintaining relationships, exercising, and so on. Frankly, comparing those who have gone through transplant to people who didn't, there are really no significant differences seen in family and peer relationships, school performance, and self-esteem is actually very well-preserved in the studies that have looked at this as well.
(36:37): Many people are going to feel anxious. I think anyone who has gone through cancer and treatment, is going to feel some concern. And sometimes relationships between the people you love most can change. I encourage having ongoing communication with your family members and taking advantage of counseling, to help ensure you are maintaining the best quality of life and relationships.
(37:08): Cognitive challenges can also occur after transplant, but only in about 19% of patients. Cognitive side-effects are actually more common after chemotherapy than in transplant. It's more common if you have other health issues, and less likely if you have a healthy social life and work environment. It’s a fine balance between avoiding crowds and people to avoid infections, and still maintaining a social life – but something worth focusing on as social interactions and relationships will help prevent cognitive decline.
(37:42): We often refer to cognitive side effects after chemotherapy as ‘chemo brain,’ and many patients want to prevent that from happening. There are many things that can be done to help combat that. Physical exercise and mental stimulation are important. Safe social interaction is very important. Mental enrichment is key. You might like to read, but you can create more complexity and diversity to stimulate your brain. Listen to audiobooks and podcasts as well as reading. Use games and puzzles to exercise cognitive functions. There's an app called ‘Lumosity’ that is great for brain exercises. Sounds like a small thing, but that diversity and mental stimulation can help clear up the potential for that chemo fog to occur
(38:48): While we’ve been talking about all the potential side effects and complications that can occur, the point of all this is to give you the tools and knowledge to help you have the best remission and quality of life after transplant possible. Don’t let fear or worry limit you. You are so much more than your diagnosis, so much more than your transplant, so much more than the process that you went through. Don't focus on the cancer that was, focus on the things that help you create a healthy future and get everything you can out of it.
(39:24): Take charge of your health and your well-being. Preventative care and early intervention means a better quality of life. Insist on communication between your healthcare providers and the transplant team. One of the best innovations has been having the electronic medical record, and many of these come with MyChart, or an online database of all of your health records that you can actually share with various medical providers. Seek help wherever you need it in order to thrive. Maintain those social connections. They may be different, but they also can be better because you are somebody who did an incredible thing.
(40:08): Reinforce healthy behaviors after treatment and look to incorporate a positive outlook and lifestyle. You are stronger than you think, and have accomplished an amazing thing that most people will never do. You have done something pretty darn amazing and that's something that you, and the people around you, should appreciate. Ask for help if you need it from your family, from your physicians, from your friends, from your counselors. And remember – You are a hero. Period.
(40:41): Summary. In summary, the number of transplant survivors are increasing, and we are working hard to ensure people are thriving post-transplant. Preventive health maintenance is the key to optimal post-transplant health, and requires a multidisciplinary team, not just your oncologist. Regular monitoring and health maintenance is all about prevention and more effective management of potential complications before they become more permanent.
(41:19): Stay engaged and participate in long-term follow-up clinics, as the protocols are there to support and promote your very best health. Patients and families who take an active role in all stages of treatment are able to ensure a healthy and vibrant lifestyle after transplant.
(41:47): I'm going to stop there and see if there are any questions that I can clarify. Thank you for your time and attention to this presentation.
Question and Answer.
(41:58): [Marla O'Keefe]: Thank you, Dr. McCarty, for this excellent presentation. Let's get to some questions.
(42:15): What are some of the problems with thyroid function that will be seen with chronic GVHD?
(42:27): [Dr. John McCarty]: You often see hypothyroidism – or a low functioning of the thyroid. Part of our long-term follow-up is to frequently check thyroid function. Graft-versus-host disease does not usually present in other ways, like Graves' disease or autoimmune thyroiditis, and we don’t expect it to happen unless someone has been exposed to radiation therapy either in that area, or potentially with total body radiation.
(43:13): [Marla O'Keefe]: Is there hope for a normal life? Going out without a mask in nature? Making travel plans?
(43:21): [Dr. John McCarty]: Once your immune system has reconstituted and you've gotten the vaccinations that you need, yes. Talk to your transplant doctor about when that time is advisable to do so, but those experiences are why we're doing your transplant and treatment. The bubble that we stay in during the time when you're at greatest risk of getting infections is to allow you to more rapidly get to where you can do the things that you want to do.
(43:50): It varies and it does take some time to give just the usual and standard vaccines. If you're going to travel to a place that might need more unusual vaccinations –like yellow fever, malaria, etc. – then I advise you to see an infectious disease specialist at a travel clinic that specializes in where you are going to be, and what you need to receive. They can discuss the pros and cons of vaccinations and prevention.
(44:26): [Marla O'Keefe]: Is strenuous exercise okay at T+180, like a 50-mile bike ride for example?
(44:36): [Dr. John McCarty]: That's a tough one. That's very individualized, and depends on where you are with the transplant, how much immune reconstitution you've done, how much your immune system is back together, what your platelets are and so on. Hopefully, you have been working your way up to that goal with less intensive exercise. Remember, this is not a great time to have a bike accident, develop road rash, and have to pick gravel out if your immune system isn't quite normal. I would double check with your doctor who knows your individual case the best.
(45:30): [Marla O'Keefe]: Will eating an anti-inflammatory diet make a difference in cardiovascular risk and do you have any thoughts on omega oils?
(45:41): [Dr. John McCarty]: I think that's probably okay. I wouldn't do that right away because some people may have a reaction. Some of the omega oils uncommonly can cause a change in liver function, so you just also want to check with the BMT pharmacist to make sure that there are no interactions with the oils and medications.
(45:58): I would say that, for example, there's also a lot of focus on the gut microbiome being a very good way of trying to improve your health, energy management and so on for your body. I encourage more than just probiotics. There are some naturally fermented foods that I often recommend – once someone’s GI tracts are sufficiently recovered –- like sauerkraut, kimchi, sourdough bread, miso soup, kombucha, a really good balsamic vinegar, and so on. In addition, you have to provide the right kind of food for the right kind of bacteria. I'm from the south, so collard greens, other greens, smashed potatoes, even “Benefiber”. Things like that provide the right kind of substrate for good bacteria to grow. All of that actually does contribute to gut health, to cardiovascular health, to metabolic health, and to immune reconstitution.
(47:35): [Marla O'Keefe]: Are you aware of any non-live vaccines being created for measles? Is there a possibility that the donor's immunity is sufficient and that the titers will come back showing some immunity for measles?
(47:52): [Dr. John McCarty]: That's actually an excellent question because that's a hot topic right now. Currently, our practice for re-immunization is at day 100 you'll get the flu and the COVID vaccination. We will give things like meningitis and the two kinds of pneumonia vaccinations around day 180. Then, once we've seen some studies that suggest that your immune system is reconstituted and you’re not experiencing graft-versus-host disease, after six months, we will do titers to see if you have protective antibodies against things like polio, tetanus, diphtheria, hepatitis, mumps, measles, and rubella. We don't vaccinate people if you have protective titers.
(48:59): We can't always predict how the transplant process is going to go. I am not aware of any non-live vaccines for mumps, measles, and rubella. It's worthwhile having a transplant infectious disease doctor to talk to. Then the decision as to when to vaccinate may really vary with whether or not there's an epidemic going on in your particular area or not. That might also change the recommendations.
(49:51): [Marla O'Keefe]: How do you know whether immune reconstitution has occurred or not?
(49:59): [Dr. John McCarty]: That's going to vary between different transplant centers, so I can only speak to ours. Some of it is age dependent – it takes a little bit longer for someone who is 65+ to get our immune system back in order compared to someone who is under the age of 30. Likewise, the age of the donor has a role in this too. With younger donors, immune reconstitution will happen a bit faster. Typically, it takes up to about six months. After day 180, our protocol is to start doing tests to see whether the immune system has reconstituted. What we focus on is whether or not your immunoglobulin (IgG) levels are ideally above 400 mg/dL unsupported. We also look at a subset of T-cells called the CD4 cells, and want levels above 250 mg/dL. When we see that those are both hitting those targets, then we feel that you're probably immune reconstituted.
(51:20): Then, we do titers to see what vaccines are needed. We have seen that if we vaccinate people too early, or if we vaccinate people with vaccines that they already have protective titer levels against, we have seen a flare in graft-versus-host disease. Different centers have different thoughts about this, and there are different studies about this, but that's what we use at our institution.
(51:59): [Marla O'Keefe]: Is it common to need two allogeneic transplants? When is it necessary and what can be done to avoid the second one?
(52:11): [Dr. John McCarty]: That's a tough one – I'm not sure that it's frequently happening – but what we're really talking about here is recurrence. The options for recurrence really depend on what the recurrence looks like, and the disease we're talking about. Is it a molecular relapse? Is it a shift in the ratio of cells being made by the donor versus the recipient (chimerisms)? Or is it a full-blown hematologic relapse where we actually can see leukemia cells or lymphoma cells or myeloma cells? Each of those are approached very differently.
(53:00): Sometimes, just dropping the immunosuppression medications, or doing them more rapidly than usual, may be sufficient enough to take care of that. Sometimes we do a ‘donor lymphocyte infusion’, where we're adding back more T-cells to the recipient, and giving back some immune system cells to see if that gets you back into remission.
(53:31): Sometimes that's not sufficient, or other times, even though we do our best to match the donor and come up with the best donor characteristics, the donor's cells can't see the cancer. Then switching to a second donor that may have a better handle on managing the transplant could be another option. It really depends on multiple factors, as I mentioned. That really is another individualized situation.
(54:08): [Marla O'Keefe]: Measles is spreading in my community. I'm still not able to be revaccinated post-transplant. Do N95 masks work for measles and how do we navigate this risk?
(54:25): [Dr. John McCarty]: I don't know. We all lived through COVID and I think you take the same kind of precautions. I don't know that I would necessarily turn into a hermit, but I would be very cautious about the public spaces. I would make sure that you have hand sanitizer. I think the best thing you can wear is an N95 when you can't control the environment. Even more generally, it's not just measles. If you have young children or are a teacher at a daycare center, if there's a plague starting to run through the group, then perhaps you wait a little bit and see what develops before coming into close contact with everyone. I think the same kind of strategies that you did to remain safe immediately after the transplant, and as we all did during COVID, would likely serve you best until we can come up with a better alternative.
(55:28): [Marla O'Keefe]: Is mowing a lawn or tilling a garden something to avoid after two and a half years after my transplant?
(55:38): [Dr. John McCarty]: That gets down to whether or not your immune system has reconstituted. If someone's immune system is still not recovered, or if you're being treated with low-level immunosuppressives, or if you have some ongoing graft-versus-host disease, you may not have as robust an immune system as your doctors would like. The concern we have about mowing lawns and tilling soils is the organic materials where fungus infections can come from. I would check with your transplant doctor, who would have a better sense of the status of your immune system.
(56:25): [Marla O'Keefe]: Thank you, Dr. McCarty, for this excellent presentation. And thank you, the audience, for your excellent questions. Please don't hesitate to contact BMT InfoNet if we can help you in any way.