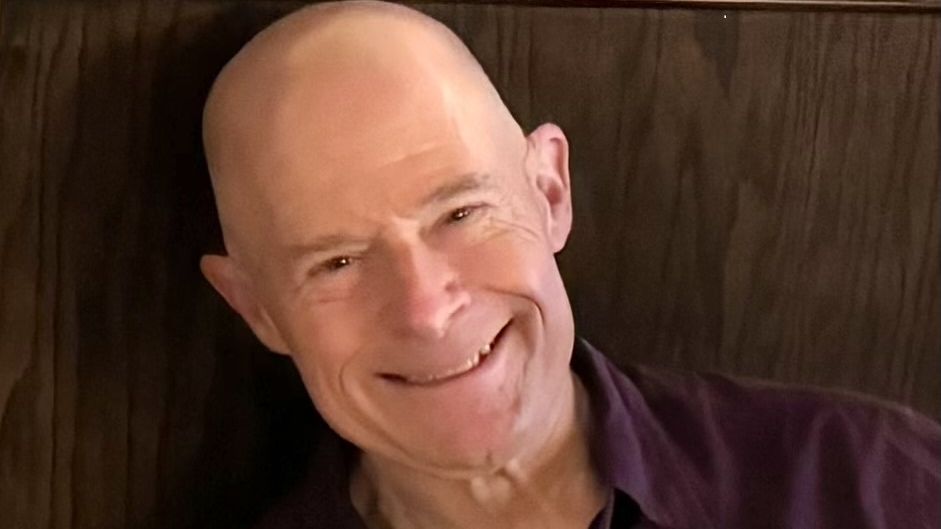
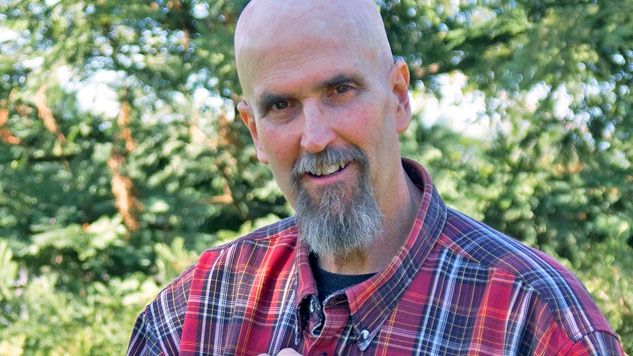
Mantle Cell Lymphoma and Acute Myeloid Leukemia: Joe and Gayle's Story
In the span of five years, Joe and Gayle were both diagnosed and transplanted. As both patients and care partners, they have lived both sides and have come through the experience stronger than ever. They remain in good health and appreciate each day.