Emotional and Psychological Effects of Stem Cell Transplants
 When confronted with the prospect of a stem cell transplant, you may still be coming to grips with the fact that you have a life-threatening illness. Deciding whether to undergo a transplant increases the emotional turmoil. Sometimes the decision must be made quickly, adding to the stress.
When confronted with the prospect of a stem cell transplant, you may still be coming to grips with the fact that you have a life-threatening illness. Deciding whether to undergo a transplant increases the emotional turmoil. Sometimes the decision must be made quickly, adding to the stress.
Managing Information
Doctors strive hard to give you a complete and honest description of the transplant experience. They want you to be fully informed about possible risks. However, the sheer volume of new information can be overwhelming.
Don’t be embarrassed to ask your doctor to repeat something or to translate it into words that you can understand. Sometimes, asking one of the nurses to explain what the doctor means will help you better understand the message.
- It helps to write down any questions you have before meeting with your doctor.
- Consider bringing a family member or friend with you to each of your appointments who can help you recall important details both before and after transplant.
- Ask to record or videotape discussions with the transplant team to help you later recall answers to questions.
- Keep a file with brochures, handouts, personal notes, and resource information in case you need to refer to them later.
Putting Things Into Perspective
For many patients, the list of possible complications is frightening. Ask your medical team to put the potential complications into perspective for you, using language you can understand.
- Which complications will definitely occur?
- Which complications happen occasionally or rarely?
- What will be done to manage complications when they arise?
- Are the complications temporary or permanent?
Don't be embarrassed to ask a question more than once until you get an answer you understand.
Doctors sometimes forget to mention that pain relief will be provided when needed. Thus, when you hear about the numerous complications that can occur, you might assume you’ll be in great pain. While there may be some painful complications associated with the transplant, there are a variety of effective pain medications and other strategies to relieve the discomfort.
Set Realistic Goals
Once you have decided to have a transplant, it's best to focus your energy on things you can control rather than dwell on those things you can't. Preparing your family for the transplant, following doctors' recommendations, and finding ways to relieve stress are ways to focus your energies on useful activities that can help with your recovery.
Ask your transplant team to help you set realistic goals during and after treatment. If your recovery takes longer than expected, don't be discouraged. A slower recovery period does not mean that the transplant is not successful. It helps to take one day at a time rather than worry about what will happen in five days, five weeks, or five years.
Be easy on yourself:
- Don't worry if you are feeling sad or discouraged. These feelings are normal.
- Don't be surprised if the coping skills you normally use to navigate problems in daily life are not sufficient to help you during transplant. You are going through a very difficult medical procedure.
- If you need help coping with your feelings, ask for it. Asking for help is a sign of wisdom, not weakness.
Anger, Anxiety, and Depression
Anxiety and distress are normal psychological effects and are an expected part of the stem cell transplant experience. These are typical reactions to a very stressful experience.
Many patients benefit from mental health services during transplant. If you need help, it does not mean you are falling apart or will require ongoing services after recovery.
You may be surprised or embarrassed if you have trouble coping with anxiety on your own. This is particularly true if you have never before sought mental health services.
A mental health provider can offer excellent ideas to help you cope with the transplant experience. Ask if there is a social worker or psychologist at your transplant center with whom you can talk or consult BMT InfoNet's Directory of Mental Health Providers.
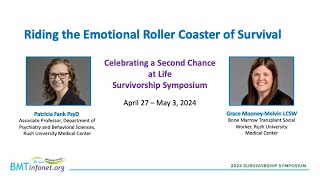
Talk With Others Who Have Been Through Transplant
You may find it helpful to talk with someone who has been through a transplant to get insights on what to expect. BMT InfoNet's Caring Connections Program can put you in touch with another person who has been through a transplant, or a person who has been the caregiver or donor for a transplant patient. Your transplant team may also be able to connect you with someone who has been through transplant.
Next Page: Preparing Family and Friends